Trust Your Gut - How To Own Your IBS
It’s estimated that 10-15% of the global population suffer from Irritable Bowel Syndrome (IBS). That’s about 1 in 10 of us who constantly worry about the consequences of our next meal. We’ve politely excused ourselves from dinner tables more times than we can count, and the idea of eating out can send shivers down our intestines.
IBS is extremely common, especially amongst women under the age of 50. And yet, every time I’ve brought up the fact that I have IBS, I’m met with the embarrassment of other people. I spare the details of course, but reactions to the mere mention of a bowel is enough to tell me that being open about my disorder is inappropriate and off-putting.
When you have IBS, the walls of your intestines contract uncontrollably if mildly triggered. This can happen if you eat too much, too little, if you eat specific foods, if you’re stressed, if you’re drunk, if you breathe…
My digestive system is high maintenance.
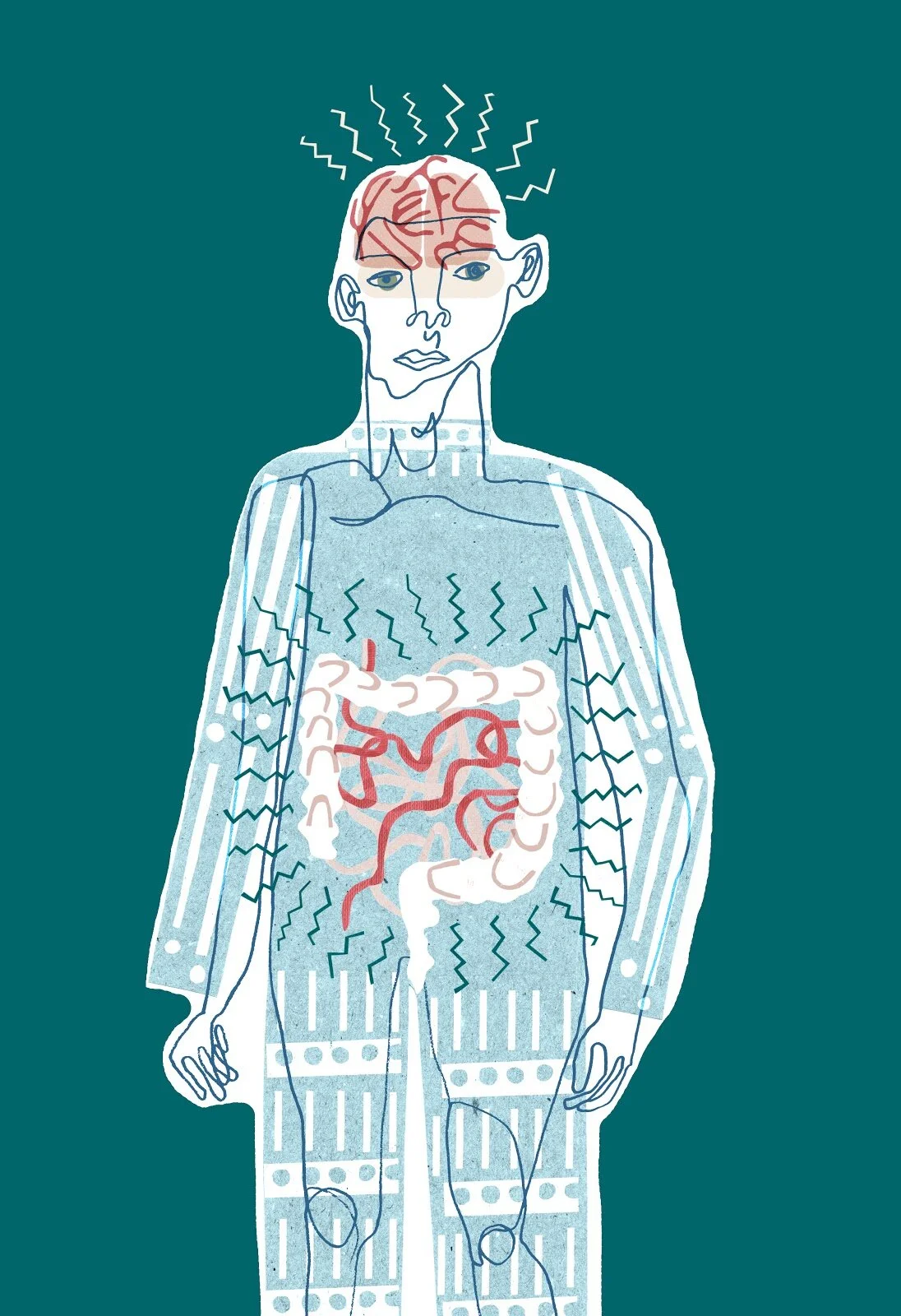
Artist credit: Becky Wakelam, A repeated print of drawings of a brain with intestines running across the image behind it.
It’s unsurprising that despite their painful experiences, only 40% of IBS sufferers seek medical help. The secrecy and shame around having IBS is extremely draining. It can completely dominate a sufferer’s life, and lead to an unhealthy relationship with food, and their mental health.
A study by Harvard Medical School is one of many about the gut-brain connection. It explains the intimate link between the human brain and the gastrointestinal system (gut).
Any strong emotions like stress, anxiety and/or depression, send signals to your gut. Therefore if your gut is extra sensitive (like mine), this means a flare up in symptoms such as: stomach cramps, trapped wind, constipation and/or diarrhea, with after effects sometimes lasting up to a week.
Similarly, if I eat certain foods that don't coordinate with my insides, my gut will send signals to my brain and can actually trigger these same strong emotions in response.
A troubled gut affects the brain, just as a troubled brain affects the gut.
Hence, if you have IBS but are continuously ignoring the needs of your digestive system, then you aren’t doing your overall well-being any flavour favours. Giving our mental and gut health some focused attention can have an overwhelmingly positive effect on our IBS, and it starts with owning it.
Artist credit: Becky Wakelam A digital drawing of a person whose brain and digestive system can be seen. There is a ring of zig-zag lines coming out from the brain at the top of the person, and a ring of zig-zag lines surrounding the person’s digestive system. The person is drawn in different shades of blue, and the background is a deep sea green.
The first thing I tried after diagnosis that eradicated some anxieties around eating was the FODMAP diet. This diet doesn’t work for everyone, however studies have shown that it helps around 85% of patients with IBS in relieving their symptoms.
FODMAP stands for Fermentable Oligo-, Di-, Mono-saccharides And Polyols: short chain carbohydrates that are resistant to digestion. These carbs are present in completely random foods, by which I mean they’re not exclusive to one ‘food type’.
Following the FODMAP diet, I avoid apples but eat oranges. Wheat, mushrooms and beans are a big no-no, but oats, carrots, and specifically the green parts of spring onions are okay.
These are just a few examples which demonstrate how the FODMAP diet is a major commitment. But in my case, it was also life-changing.
Rather than viewing the FODMAP diet as an inconvenience, label it an act of self-love. If we treat our body with care and nurture, our overall mood improves and we have more confidence approaching foody situations.
After just one month of trying the diet, I could finally enjoy the feeling of being full again, without the smell of impending doom lingering over my plate.
There’s a great resource for learning more about the FODMAP diet here, and I strongly recommend Gastroenterology Dietitian Lucy Wigham’s low-FODMAP recipe book for preparing gut-friendly meals at home. (Disclaimer: make sure to contact your GP first before trying the FODMAP diet).
Whether you’re taking or leaving the above advice, you’ll hopefully resonate with some of my following tips for owning your IBS:
Meditate through your dips. There’s a fantastic episode of Headspace: Guide to Meditation that looks at dealing with physical pain. I’ve found it extremely useful when working through prolonged, house-bounding stomach aches.
Avoid tight waistbands. “But skinny jeans look great on me!” And so does that radiant smile you’ll be flashing everyday when not pressing unnecessary pressure on your internal organs. Elasticated anything is my go-to style.
Know your cycle. People who menstruate may find their symptoms flaring up during their period. Avoid the foods you definitely can’t handle in the lead up to and duration of your bleed.
Worship your well-being when out and about. There is zero shame in tapping out of an event because your IBS is being an attention-seeker.
Trust your gut. Sometimes a bite of that Gregg’s steak bake isn’t worth it, and yet, we’re only human. If you find yourself suffering from your moment of weakness, please, go easy on yourself. IBS is ruthless, but it doesn’t always have to win.
Read more about diagnosis and treatment of IBS on the healthline website.
Written by Annabel Chadwick
With images by Becky Wakelam